Illustration by Gracia Lam
The social prescription
How social interventions could help us live healthily for longer.
How do we care for an aging population without overwhelming the hospitals, clinics, and providers already stretched to their limits? Is medical intervention the only option—treat the illness, manage the decline, hope for the best?
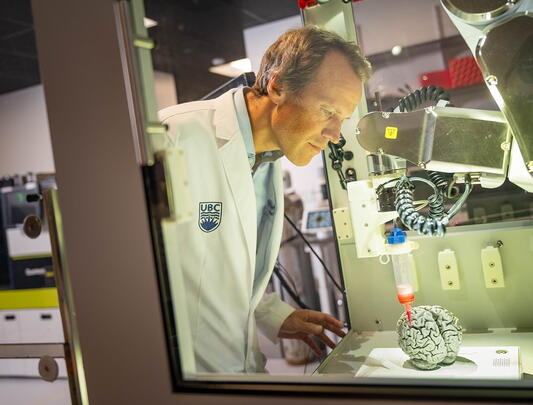
In the United Kingdom, “social prescribing” has long served as a complement to medical intervention in the aging community, a concept recently imported to Canada that focuses not just on prescriptions, but on people. “Social prescribing is a way of connecting the health system with community services,” says Dr. Grace Park, clinical professor in UBC’s Faculty of Medicine and past medical director for Home and Community Care at Fraser Health. “It provides a pathway for the healthcare provider to refer their patients for non-medical issues.”
Some factors of age decline aren’t visible in a clinical chart, but have a profound effect on health and wellbeing. Addressing needs like transportation, food security, housing, and social isolation can mean the difference between older adults staying independent and needing institutional care. “It could be something unrelated to their health concerns, but often does end up having an impact on their health,” adds Dr. Park. “It could be they can’t afford rent anymore. Or they can’t get to the grocery stores, or they have issues with isolation and loneliness, and they have nobody to call if they have problems.”
This holistic approach to age-related care started in British Columbia as a pilot program in 2019, with funding from the Ministry of Health through United Way BC. Fraser Health served as a demonstration site, launching social prescribing programs at 10 community organizations with the help of newly created roles called “community connectors.”
“The connectors will speak to the older adult and find out what's going on in their lives, what the biggest issues are,” says Dr. Park. Since the program began, nearly 3,000 referrals have been made in Fraser Health alone, and more than 100 community connector positions have now been funded across the province. And because the system is integrated with electronic medical records, referrals can come from family doctors, emergency departments, and even hospital pre-op clinics—anywhere a practitioner identifies unmet social needs for older adults.
“We recently had a program at Peace Arch Hospital in White Rock,” Dr. Park says. “Patients that were coming in for elective surgery—mostly hip and knee replacements—were assessed for surgical optimization, including social prescribing. The surgeons were really surprised this program was in place. They felt that the volunteers from the community organizations were angels, driving people to doctor’s appointments, bringing them food, picking up their meds.”
some factors of age decline aren’t visible in a clinical chart, but have a profound effect on health and wellbeing. addressing needs like transportation, food security, housing, and social isolation can mean the difference between older adults staying independent and needing institutional care.
Some patients may only need a one-time referral—help with finding a new apartment, a culturally appropriate exercise program, or a hot meal. Others, especially those who are frail or isolated, may receive ongoing follow-up, with community connectors or volunteers calling regularly, making home visits, or connecting them to additional health authority services like home support and personal care.
By addressing the root causes of vulnerability earlier, the system can help people live independently for longer. “What we want to do is get in there before they’ve gotten to that point where they need extra care from the health authority,” Dr. Park says, “and really support them so that they can remain as active and healthy as possible. So we’re doing upstream preventative work, and doing it in a holistic way by addressing the social determinants of health.”
The rewards extend beyond the health of the individual; social prescribing is an important support system for caregivers, helping to prevent the burnout that comes with constant attention to a loved one’s needs. And as Canada moves closer to the UK model, where social prescriptions are applied to all ages as part of their comprehensive Universal Personalized Care program, the economic incentives will keep pace with the benefits to individuals. According to the Canadian Institute for Social Prescribing (CISP), every dollar invested in social prescribing programs already brings a return of up to $4.43 through improved wellbeing and reduced costs to the healthcare system.
“I think increasingly it is going to become part of general practice and hopefully part of healthcare in general,” says Dr. Park. “We want to have it as integrated as possible, so it becomes a normal part of practice when we’re dealing with medical issues, addressing some of the deficits patients might have in their social determinants of health, and making those connections in the community.”