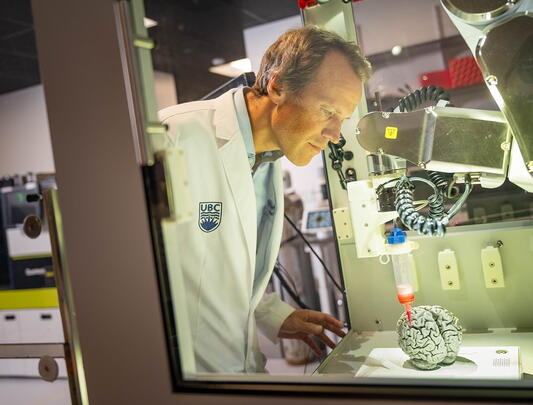
UBC emeritus professor of sociology Dr. Anne Martin-Matthews. Photo by Martin Dee.
Are we prepared for an aging world?
Aging populations are a societal achievement, says UBC sociologist, but sustaining them requires new ways of living, working, and caring.
Here’s the good news: It’s highly likely that most of us will live much longer than previous generations. And here’s the complication: During all those bonus years, we’re going to be “elderly,” a state of being that is loosely defined and poorly understood. Given that a daunting percentage of us are all about to be elderly at the same time, it’s also a state for which our society is surprisingly unprepared.
That’s the news as filtered through the long lens of UBC emeritus professor of sociology Anne Martin-Matthews. Dr. Martin-Matthews has been an avid student of the sociology of aging since pursuing her MA and PhD at McMaster University. In Hamilton she discovered the inspirational Dr. Victor Marshall, who in 1971 co-founded the Canadian Association of Gerontology. She also happened to be rooming with an elderly widow to whom she grew close. The pieces fit to spark her interest and form the foundation of a long career in the field, of which she is now a respected elder.
For example, while scientific director of the Institute of Aging of the Canadian Institutes of Health Research, Dr. Martin-Matthews led the strategic development of the Canadian Longitudinal Study on Aging (CLSA). Launched in 2010, the study is following over 50,000 participants aged 45 to 85 at recruitment for 20 years. The data collected, says the CLSA, is “allowing researchers to answer critical questions on the biological, medical, psychological, social, lifestyle and economic aspects of aging, disability and disease.”
Now 74, Dr. Martin-Matthews finds herself in the midst of the population she has been studying her whole career: “I have become what I have been teaching.” It is, she says, a moment of great professional fascination, and she quotes the Oregon State University gerontologist Jon Hendricks, who wrote in a 2008 paper, “Those of us who study aging have the unique opportunity to live their subject matter,” adding that “personal experience can make us far better scholars than can scholarship alone.”
But even up close the subject is elusive, says Dr. Martin-Matthews, beginning with the word “elderly,” which she calls “an ultimately meaningless term, homogenizing an entire population that can span 30 to 40 years or more.” The statistics are on her side. In 1900, the average life expectancy in the world was 32, and in Canada about 50. Yet the United Nations reported in the UN Decade of Healthy Ageing (2021-2030) that people who turned 60 at the start of the decade could expect to live another 22 years. And that’s a global average. For an increasing number of citizens in privileged democracies, it could be another 30 or 40 years. In their 2016 book, The 100-Year Life, London Business School professors Lynda Gratton and Andrew J. Scott estimate that babies who were born in 2011 have a one in three chance of living to 100 if they are female and a one in four chance if male. As Dr. Martin-Matthews says, “It becomes a substantial proportion of your lifespan.”
On an individual basis, the additional years sound positive. But as the Baby Boom bulges into that elderly demographic—and as birthrates decline sharply in developed countries—the fact of population aging comes with significant social implications. Globally, the number of people over 60 is expected to comprise 22 per cent of the world population by 2050, up to 2.1 billion from 1.4 billion today. And well over 400 million of them will be over 80. Without an equal or larger population of younger people to work, pay taxes, and provide care for those elders, there could be an insupportable strain not just on the social safety net, but on the global economy.
Stats Canada projects the number of people over 65 in this country could climb to more than 11 million over the next 25 years under a medium-growth scenario—almost one quarter of our population.
Dr. Martin-Matthews says there is a looming crisis in the funding of Canadian healthcare and a lack of preparation for population aging at the societal level. Cancer is one example—a disease that increases in prevalence with age and is expensive to treat. On this topic, she refers to the journalism and advocacy of Globe and Mail health columnist André Picard, who wrote in 2023, “The Baby Boom started more than six decades ago. That the incidence of cancer would grow has been widely known for years. At some point, we have to stop pretending that the aging of the population, and the shift in care that needs to accompany it, are a surprise. We have to be aggressively proactive, not pitifully reactive.”
Of course, the very fact of an aging population attests to the progress already made in pursuit of healthy aging, both from technological advancement and from improvements in preventative care. Even while the healthcare system—and many researchers—continue to focus on treatment and cures for sickness and disease, there has been increased attention on the gains that can be made from lifestyle choices and from tracking the social determinants of health.
Dr. Martin-Matthews says there are definitely solutions, as modelled in countries such as Denmark and Finland, which are making progress in the creative provision of home care. In Denmark, for example, homecare workers traditionally offer home visits twice a year to everyone over 75. Even if some people do not need a visit, this population-based approach allows care providers to identify broad issues and to actually reduce health expenses by heading off unanticipated problems.
But, Dr. Martin-Matthews says, the potential responses are tough in Canada. Unlike Australia, New Zealand, or most countries in Europe, healthcare delivery in Canada is divided up among 13 provincial and territorial jurisdictions. This contributes to an environment full of research and innovative ideas, but often little capacity to turn them into active policy solutions. For a deeper explanation of that failing, Dr. Martin-Matthews invokes the former federal minister of health Monique Bégin, who co-wrote a 2009 article in the Canadian Medical Association Journal, saying: “When it comes to moving healthcare practices forward efficiently, Canada is a country of perpetual pilot projects. We seldom move proven projects into stable, funded programs, and we rarely transfer the outcomes of pilot projects across jurisdictions.”
“‘Elderly’ is an ultimately meaningless term, homogenizing an entire population that can span 30 to 40 years or more.”
~Dr. Anne Martin-Matthews
On the larger question, though, of whether an aging population constitutes a crisis or an opportunity—even “a societal achievement”—Dr. Martin-Matthews says, “An age-friendly society is better for people of all ages.” Aside from setting a more humane example for the whole population, she points out that accommodations or protections that serve older people are also there to benefit everyone else. On the mobility front, for example, she says that better accessibility on public transit helps everyone who can’t or doesn’t want to drive; curb cuts on sidewalks for older people or wheelchair users benefit parents with baby buggies; and longer lights at intersections allow the old and the young a better chance of making it to safety before the light turns red.
On the prospect of aging itself, Dr. Martin-Matthews is an optimist, at the ready with reasons for facing later life with less trepidation. For example, she points out the common view that dementia cases are increasing, which is true in hard numbers precisely because the number of older people is increasing. But, she says, there has actually been a decline in the proportion of older people with dementia worldwide.
This trend is most pronounced in wealthy countries: Harvard University research has shown that over the past 30 years, the likelihood of dementia in people of European ancestry living in the United States and Europe has declined an average of 13 per cent every decade, likely thanks to improved healthcare and nutrition.
There are also age-related issues like retirement. While some people are eager to leave the workforce early (and want their retirement benefits assured), others are happy in their jobs and don’t want to be pushed out the door. Dr. Martin-Matthews points out that the move against mandatory retirement came not from employers who wanted to keep workers at their tasks, nor from governments or pension funds trying to delay payment, but from workers who wanted to stay in their jobs. Specifically, a group of UBC professors fought their case all the way to the Supreme Court of Canada, which ruled in 1990 that the university’s mandatory retirement policy was unconstitutional. However, the court also ruled that the policy was a reasonable limit to the Charter of Rights and Freedoms, and it stayed in place until 2010, when BC finally prohibited age discrimination in employment. Today, an increasing number of healthy people in the growing older demographic can continue making a contribution, rather than being forced into inactivity.
Globally, researchers and policy-makers are also seeing a silver lining in the workforce participation of a healthy older cohort. A recent research paper for the International Monetary Fund suggests: “Healthier aging could… boost labor supply by extending working lives and enhancing older workers’ productivity, offering a bright spot amid the rise of the silver economy.” For example, the IMF reports, “Data from a sample of 41 advanced and emerging market economies indicate that, on average, a person who was 70 in 2022 had the same cognitive ability as a 53-year-old in 2000.” That change has led to a 20 per cent increased likelihood that individuals will stay in the labour market, with an average six-hour weekly increase in time worked and a 30 per cent rise in labour earnings.
Dr. Martin-Matthews herself took retirement last year, but, she says, “It’s mostly a change of my financial relationship with the university.” That is, like other people of a certain age who aren’t keen to give up jobs they love, she is still working on initiatives of interest to her—still eager to contribute—but no longer being paid as before. Dr. Martin-Matthews is okay with that transition, which she says is not so much a retirement as a “rewirement.” She gets to adjust her pace but still embrace a hard-earned opportunity to live out the details of her academic study, and take advantage of a new and more intimately informed perspective.
In that regard, Dr. Martin-Matthews says she has always been fond of a quote attributed to the philosopher Søren Kierkegaard: “Life can only be understood backwards; but it must be lived forwards.” Now, though, she gets to edit Kierkegaard, at least to the extent that she can look back critically and more knowledgeably on her own research to see what she might not have seen before, and to use her personal experiences to help identify gaps in theory and practice—ultimately, “to understand our aging.”