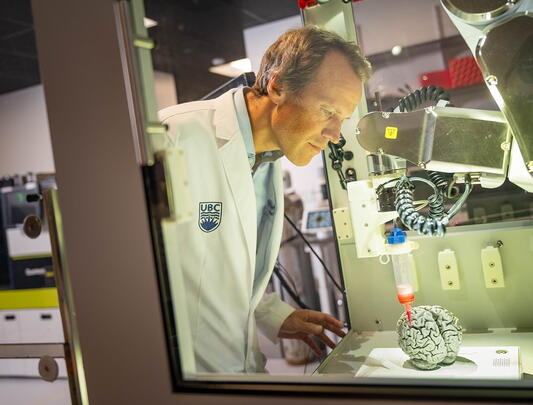
Dr. Pieter Cullis
Saving the world, one bubble at a time
The most widely used COVID vaccine relies on a novel drug delivery system developed at UBC.
On a chilly morning in late March, 2021, Dr. Pieter Cullis left his lab on the fifth floor of UBC’s Health Sciences Building, took an elevator to ground level, and crossed the street to the COVID-19 vaccination clinic in Pharmaceutical Sciences. There was nothing outwardly remarkable about this brief walk, yet to 75-year-old Cullis it felt like the journey of a lifetime.
“I had something to do with how this vaccine came into being,” he told the nurse, as she prepared to jab him with a dose of Pfizer’s COVID vaccine, but the look on her face betrayed disbelief, and he said no more.
An imposing figure who bears a notable resemblance to Mick Jagger, Cullis has been a fixture on the UBC campus nearly all his adult life. Initially, he followed in the footsteps of his father, a physics teacher, but after graduating from UBC with both a BSc and PhD in physics he made a daring transition, chasing down a postdoctoral fellowship in biochemistry at Oxford. He had the idea to study biological membranes using a technique from physics called nuclear magnetic resonance. Biological membranes are comprised primarily of lipids and proteins. “I didn’t know the language they were speaking,” he says. “I didn’t know what a protein was, or DNA. For a couple of years, I felt like the emperor with no clothes.” Looking back on it, though, he wouldn’t change a thing. “It’s a big advantage to switch fields,” he says. “It gives you a lot of confidence that you can try the next thing.”
“I didn’t know what a protein was, or DNA. For a couple of years, I felt like the emperor with no clothes.”
After completing his postdoctoral work, he returned to UBC where he has dedicated his entire career to the study of lipids (fat-soluble molecules utilized by living cells). He pioneered research on fashioning microscopic lipid bubbles, now known as lipid nanoparticles or LNPs. These remarkable particles are able to carry drugs to diseased tissues in the body, and release their cargo precisely where most needed.
Cullis was always interested in therapeutics, but to put a drug through clinical trials can easily cost $100 million. For this, investors are needed, and to attract investors one needs a company. In the early eighties, young Cullis had no idea how to set up a company, but his switch from physics to biochemistry had made him bold. “I’ll start one anyway,” he told himself, and over the years has started more than 10.
Together with five senior scientists in his UBC lab, he co-founded his first company, Lipex Biomembranes. “Pieter had an idea about how to make LNPs quickly, taking minutes rather than days, and he designed a device to do it,” relates friend and co-founder Dr. Michael Hope, whose garage served as the company’s production centre. The invention facilitated rapid testing of therapeutics, and mass production of pure LNPs of any desired size. “We named the device ‘The Extruder’,” Hope says, “and sold thousands.”
In the early eighties, young Cullis had no idea how to set up a company, but his switch from physics to biochemistry had made him bold. “I’ll start one anyway,” he told himself, and over the years has started more than 10.
Because companies should have mission statements, they made up one for Lipex Biomembranes: Free beer every Friday and parties whenever possible. “Nobody in my lab has ever had to pay for beer on a Friday since then. That convinced us that starting companies was a good idea,” quips Cullis, only partly joking. He is known for his ability to rally people and keep them motivated and enthusiastic by taking them out for parties and dinners and beers.
Countless top-notch teams of graduate students and postdocs have passed through the Cullis lab at UBC, contributing research essential to innovative applications. Once their academic journey is completed, they yearn to apply their expertise. “It’s a terrific reason for starting a company – so you can keep that team together,” Cullis says.
In the 1980s and early 90s, when lipid delivery systems were still what he calls a “fringe field,” he was devising ways to load anti-cancer drugs into LNPs to deliver them directly into cancerous tissue, making the treatments more focused and efficient than conventional chemotherapy while triggering fewer side-effects.
Then, in 1995, he began developing LNPs to encapsulate nucleic acid medicines – made of RNA or DNA – which were at the cutting edge of therapeutic research. In order for these treatments to function in humans, researchers had to overcome two massive hurdles.
The first hurdle was to synthesize the RNA in such a way that the body’s immune system would not reject it, a dilemma a number of other scientists were striving to resolve. Notable among these others was a determined woman at UPenn, Dr. Katalin Karikó. Long a voice in the wilderness proclaiming the limitless potential of messenger RNA (mRNA) to treat, prevent, or cure just about any human disease, Karikó would one day enter into a significant partnership with a UBC spin-off co-founded by Cullis. The second hurdle was at the core of Cullis’s research: how to get nucleic acids safely to their destination in the body.
In 2004, following nine years of research on LNPs for RNA and DNA, Cullis shared his results at a conference in London. Immediately, a drug company pursued him. They had a molecule, patisiran, made of short interfering RNA (siRNA) to treat transthyretin-mediated amyloidosis, a fatal condition affecting 50,000 people worldwide, but there was one problem: they lacked a way to get their drug into the hepatocyte cells in the liver. Would Cullis design an LNP delivery system for patisiran? The Cullis UBC lab along with two Cullis-affiliated companies – Inex Pharmaceuticals and, subsequently, Acuitas Therapeutics – took up the challenge.
Acuitas has just 29 employees but its accomplishments are impressive. By 2012, they had refined the LNP for the siRNA drug, patisiran, and it was ready for human clinical trials. Then the team set themselves a new challenge, developing LNPs to hold mRNA. The least stable of all RNAs, mRNA is also very large – orders of magnitude larger than cancer meds, for example – so the LNPs carrying it must be specially designed. Furthermore, the lipid carrier must access the cell cytoplasm, and, once there, release its cargo. Lastly, it must be nontoxic. Each of these tall orders has been the focus of decades of research and experimentation by a great many scientists. In many ways, Cullis has led the pack.
In 2014, Acuitas’s work on mRNA encapsulation caught the attention of Dr. Drew Weissman, an American immunologist who had partnered with Dr. Karikó, now an executive with the German research company, BioNTech. Weissman and Karikó had worked out how to synthesize mRNA vaccines for human therapeutics, but were still without a suitable delivery system for the vaccines. Weissman asked Acuitas for help. “We packaged up some of his messenger RNA that was coding for a protein on a virus,” Cullis says, “and it worked brilliantly well as a vaccine.” Neither the team at Acuitas, nor Weissman, nor Kariko at BioNTech had any inkling of the mind-bending impact their partnership would soon have on lives around the globe.
Weissman and Karikó had worked out how to synthesize mRNA vaccines for human therapeutics, but were still without a suitable delivery system for the vaccines. Weissman asked Acuitas for help.
Meanwhile, patisiran proved effective, halting and even reversing the progress of transthyretin-mediated amyloidosis. In 2018, after six years of clinical testing, the United States Food and Drug Administration (FDA) approved its use. The culmination of 40 years of research and technological innovation in Cullis’s UBC lab and its spin-off companies, this was a ground-breaking double achievement: the first-ever LNP drug approved by the FDA, and the first FDA-approved medicine comprised of RNA.
This landmark victory for science coupled with the thrill of contributing to life-saving technology would be a career high point for almost any scientist and, for a septuagenarian like Cullis, might signal the perfect moment to retire. But he was not about to ride off into the sunset, and still isn’t. Nor, as it turns out, was he anywhere near the high point of his career.
When the novel coronavirus became a global health emergency in January 2020, Acuitas and BioNTech (which quickly partnered with Pfizer) pivoted from influenza vaccines to COVID-19 vaccines. Because both these vaccines are made of mRNA, they need similar LNPs. Still, the team at Acuitas worked days, nights, and weekends until they had optimized an LNP specific to the COVID-19 vaccine.
Three months later, 43,000 volunteers were recruited for the vaccine’s clinical trials, conducted in accordance with the FDA’s rigorous standards. On November 8, 2020, Pfizer released results indicating 95 per cent efficacy. “It was hard to absorb,” Cullis says. “You spend all your life hoping for a great outcome of one form or another, but one comes along like that! I think I literally sat here for an hour, just thinking ‘Wow! This is something else!’ Then calling everybody up and saying we’ve got to have a celebration.”
The Pfizer/BioNTech COVID-19 vaccine was the first one approved for emergency use in Canada and is the most widely used in the world. While Cullis insists that hundreds of scientists, perhaps thousands, contributed to the success of this vaccine, much of the credit belongs to the team at Acuitas. As UBC’s Dean of Medicine Dermot Kelleher said on GlobalNews: “The development from UBC of the nanoparticle encapsulation is the critical factor that allows that vaccine to work.”
“It was hard to absorb,” Cullis says. “You spend all your life hoping for a great outcome of one form or another, but one comes along like that! I think I literally sat here for an hour, just thinking ‘Wow! This is something else!’ Then calling everybody up and saying we’ve got to have a celebration.”
It takes immense energy to teach classes, run a lab, or build a company, but doing all three at once, as Cullis has often done, takes exceptional stamina. It should come as no surprise, then, to learn of his athleticism. A lifelong runner until a knee injury put a stop to that a few years back, he was also a regular on “the circuit,” which colleague Michael Hope describes as “a series of exercise stations around the top tier of the War Memorial Gym where you did different intense exercises at each station, lifting weights etc. I could not keep up with him.”
These days, if he isn’t at the gym lifting weights or cross-training, Cullis may be found leading graduate students in a seminar, or participating in a conference via Zoom, or mobilizing RNA in his lab to conquer what may be the most daunting terrain of all: “When we get these kinds of therapeutics to the brain, then everything from Alzheimer’s to Huntington’s to Parkinson’s, every disorder you care to name, comes into focus,” he says. “That’s where we push things in the university environment – that really exploratory stuff.”