Illustration by Gracia Lam.
Mind games
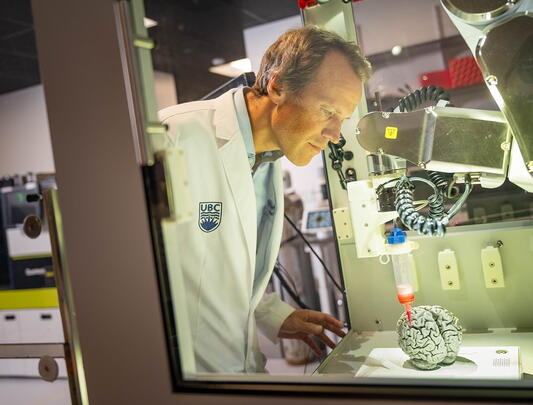
Virtual Reality has the power to transport a user’s mind to an infinite number of places and scenarios, but is it powerful enough to block out external pain? Nursing prof Bernie Garrett discusses the technology’s potential.
What is the theory behind VR’s ability to relieve pain?
We know the brain can suppress pain by modifying sensory input. A good illustration of this is that if you have more than one type of pain — both knee and hip pain, for example — you tend to only focus on one of them at a time, as neural pain attenuation tends to work in a prioritizing manner. Virtual Reality is a deeply immersive experience and essentially works as a very powerful form of distraction. It transports you to a computer-generated beach or forest — anywhere we want — and the immersion is so complete you can hear a bird tweeting, look in its direction, and see it as you move around. Although the graphics may not be as high fidelity as in real life, they are convincing enough to make you perceive you are actually there. Having the patient perform therapeutically designed activities in a VR environment forces their brain to focus on something other than the pain and allows them to get some relief from it.
How has it proven effective?
There is far more research on acute pain than on chronic pain. It’s been shown to work well for burn patients having dressings changed, for example, immersing them in cold or snowy virtual environments that psychologically reduce the heat and pain. It’s also been shown to help when giving kids injections, and I imagine in five years’ time most pediatric clinics will have a VR headset they can use to distract kids during those sorts of procedures. For chronic pain, the results are still mixed, but it does seem to work well for some things, such as phantom limb pain. In fact, VR is becoming a standard therapy for this, providing experiences where the patient sees both limbs working. This seems to have a profound effect on the brain and a person’s experience of pain.

Describe your current research
Chronic pain is a huge issue in Canada affecting millions of people, and it's not well managed in the health system. As nurses, we're very interested in practical applications of technologies in healthcare, so we are using VR in the homes of cancer patients with chronic pain who have been on opioids long term to see if we can help alleviate their pain in other ways. We’re giving them VR headsets to use for a month and measuring their pain scores, sleep index and functional ability. A control group is viewing the same applications, but on a computer screen instead of in VR. Most pain-related VR research tends to occur in clinics and address acute pain. We’re the first to conduct trials in people's homes and explore VR’s use as a daily pain reduction tool.
What are the cancer patients experiencing in VR to help alleviate their pain?
We have four VR applications. Two are cognitive, requiring patients to problem-solve. For example, one involves navigating a three-dimensional light maze by manoeuvring mirrors to move light beams. Such spatial problem-solving involves a lot of high-level cognitive activity. The other two applications offer more introspective experiences — for example, a guided meditation experience while walking through a forest.
What have you discovered so far?
COVID-19 restrictions mean the trials are on hold, but, as soon as we are able to recruit enough participants, we will have a good sense of whether the VR is making a difference in terms of their pain. So far, electroencephalogram (EEG) studies have shown some distinct patterns. These include changes in the brain’s alpha-theta bandwidths, areas usually associated with more inward-attentive and reflective activity.
Could VR therapy replace pharmaceutical pain relief?
At the moment, we're exploring it as an adjunctive therapy. Many patients with chronic pain are taking opioids, which are powerful narcotics with side effects, so anything we can do to reduce the amount they need is helpful. Also, patients can only tolerate VR for about 30 minutes, after which they can get eye strain and neck ache. So, people get a pain holiday for half an hour, but in terms of continual use we're not at the stage where we can use VR to supplant drugs. New technologies being developed that use projected VR environments instead of a headset could eliminate these limits. They would also permit more detailed neurological studies, such as MRI scans of the brain during a VR experience — currently impossible because of the metal in headsets.
Research Participants Needed
The researchers are recruiting cancer outpatients who are over 16 and experiencing moderate to severe daily pain. For more information, contact Crystal Sun, UBC School of Nursing, 604-822-7679 / crystal.sun@ubc.ca.