Illustrations by Naíma Almeida
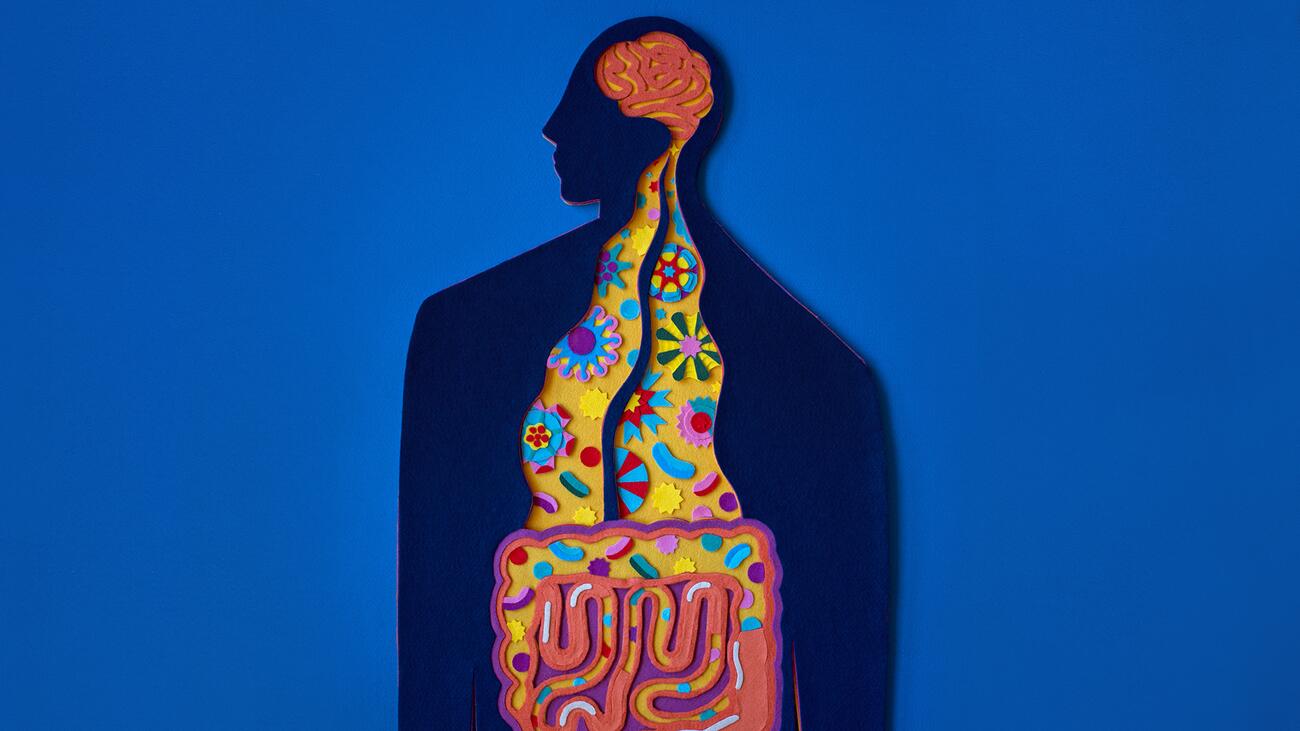
Our second brain: More than a gut feeling
The human gut contains more nerve cells than the spinal cord and exerts significant influence on the brain.
You don’t need a degree in neuroscience to suspect that the brain and gut are somehow connected. The feeling of “butterflies” in our stomach when we prepare to give a presentation, stress-induced stomach ulcers, emotional eating, and even our intuition showing up in the form of a “gut feeling,” all provide clues that the brain and gut are talking to each other.
But the brain and gut are far more connected than most of us realize. In fact, emerging evidence is showing that the gut-brain axis is one of the most powerful relationships in our body.
Our Enteric Nervous System
Comprised of 100 million neurons, the network of nerve cells lining the digestive tract is so extensive that it is sometimes called the “second brain.” Technically known as the enteric nervous system, this network of neurons is often overlooked – yet it contains more nerve cells than the spinal cord or peripheral nervous system.
This resemblance to the brain in our heads doesn’t end with neurons. The mass of neural tissue in our gut produces over 30 different neurotransmitters, which are signalling molecules typically associated with the brain. This includes a staggering 95 per cent of the production and storage of serotonin, the neurotransmitter famously known as the “happy chemical” due to its role in regulating mood and wellbeing.
Gut-Brain Crosstalk
So how do the brain and gut actually talk to each other? A thick cable of neurons runs between the base of the brain and our gut forming the vagus nerve, the longest cranial nerve in our body. The vagus nerve serves as a bidirectional information highway, with the brain and gut sending messages to each other within the order of milliseconds.
The vagus nerve isn’t the only way the brain and gut communicate. Our guts are home to trillions of bacteria and microbes that inhabit the intestines and form the gut microbiota. The gut microbiome is so enormous that there are 100,000 times more microbes in your gut than there are people on Earth.
Many of these microbes live in the mucus layer that lines the intestines, placing them in direct contact with nerve and immune cells, which are the major information gathering systems of our bodies. This location also primes microbes to listen in as the brain signals stress, anxiety, or even happiness along the vagus nerve.
But the microbes in our gut microbiome don’t just listen. These cells produce modulating signals that send information back up to the brain. In fact, 90 per cent of the neurons in the vagus nerve are actually carrying information from the gut to the brain, not the other way around. This means the signals generated in the gut can massively influence the brain.
The vagus nerve serves as a bidirectional information highway, with the brain and gut sending messages to each other within the order of milliseconds.
The Influence of Gut Health on Brain Health
The crosstalk along the gut-brain axis helps make sense of the accumulating evidence that the gut is involved in brain health and disease. Many neurological conditions, such as Parkinson’s disease, Alzheimer’s disease, schizophrenia, and autism spectrum disorder are correlated with gastrointestinal issues or altered gut microbiomes.
Recent research on Parkinson’s disease found that the enteric nervous system begins to degenerate before the classical symptoms of Parkinson’s appear, and a dysfunctional gut microbiome is typical of this disease. Further, there is a significant decrease in the quantity of microbes in the gut microbiome of individuals with Alzheimer’s disease, and an unhealthy diet is a commonly cited risk factor for Alzheimer’s.
One explanation for this is the role of inflammation, which is a chronic symptom in many neurological conditions. Disruption in the health of the gut microbiome can trigger an immune response and lead to inflammation. Over 70 per cent of the body’s immune cells are targeted to the digestive tract – which is helpful in the case of ingesting toxic bacteria but also means a gut-immune response can launch a powerful inflammatory response in the body.
The Role of the Second Brain in Mood Disorders
Inflammation is also a hallmark of mental illness and may explain the link between gut and mental health. For example, a recent study reported that a significant number of patients with inflammatory bowel disease also suffered from depression and anxiety.
Both the vagus nerve and gut microbiota are likely involved in this. Stimulation of the vagus nerve has been shown to reduce inflammation and stress, and some researchers are even suggesting that vagus stimulation could be a new drug-free antidepressant. Certain healthy gut bugs like the probiotic Lactobacillus rhamnosus, can even send signals to neurons to release GABA, a neurotransmitter sthat promotes calmness. Gut microbes also promote neuroplasticity, a process implicated in mood.
While it is now apparent that the gut is more than just a machine for digesting food, there is still much to be discovered in terms of how the gut can influence overall health. As our understanding of the gut-brain axis increases, there is the exciting possibility that improving gut health may lead to breakthroughs for treating brain disorders.
The Gut-Brain Axis
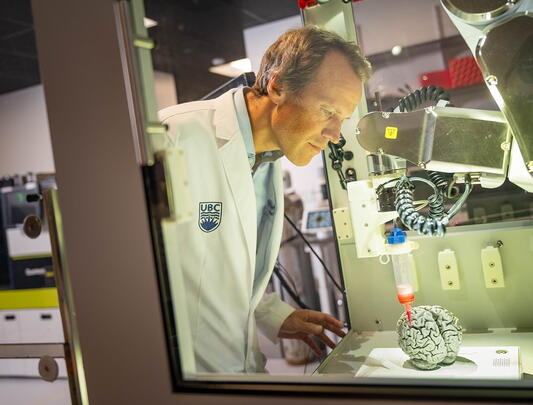
UBC researchers are uncovering the links between gut health and brain health
Modern life and missing microbes
Carolina Tropini’s Favourite Brain Food: Berries (which are high in antioxidants)
Dr. Carolina Tropini (BSc’08) is an assistant professor in the School of Biomedical Engineering and Department of Microbiology and Immunology. Her research examines how industrialization and modern lifestyles have led to the loss of key bacteria from our gut microbiota and the impact of this on human health and disease.
But how do you go about establishing which microbes have been lost? Tropini’s team compared the microbiomes of people from traditional and industrialized societies and noted which microbes were missing from the industrialized gut. Modern lifestyle factors such as antibiotic usage, diets high in processed food, increased sanitization, and less time outdoors have reduced exposure to bacteria and changed the landscape of the gut microbiome. “In turn, an altered microbiota increases risk for modern diseases such as chronic inflammation, diabetes, and inflammatory bowel disease [IBD],” says Tropini, “all of which were unknown to our ancestors.”
Tropini’s lab has a growing interest in how early-life gut inflammation influences the developing brain. In a collaborative project with Dr. Annie Ciernia, co-winner of the UBC Faculty of Medicine 2021/2022 Precision Health Catalyst Grant, Tropini’s team induced gut inflammation in young mice to mimic pediatric IBD. These young IBD mice demonstrated abnormal immune signalling in the brain, alongside deficits in social and cognitive development.
Untangling the implications of a depleted microbiome on brain health beyond development is a work in progress. “There is a lot of correlation between altered gut microbiota with inflammation, which leads to an increased risk of depression and dementia,” says Tropini. But she notes, “Eating poorly for one meal likely won't lead to permanent negative impact; it’s lifestyle changes and loss of these microbes that can cause long-term effects.”
What can we do to regain healthy microbes in our gut once they’ve been lost? The answer may not be quite as simple as a probiotic supplement. “Not all probiotics are created equal,” explains Tropini. Fermented foods such as yogurt, kimchi, and sauerkraut are more helpful for building resilient immune systems because they create a natural exposure to microbes. “If you want to reintroduce bacteria there need to be things in place that will support natural growth and integration.” Tips for creating a supportive gut environment include a diet with plenty of variety and fibre to help different members of the microbiota flourish.

Could a parasitic worm help MS patients?
Lisa Osborne’s Favourite Brain Food: Coffee (which can be protective against Alzheimer’s)
The thought of a parasitic worm living in your gut is generally not a positive one. But Dr. Lisa Osborne (PhD’11), an associate professor in the Department of Microbiology and Immunology, is on a mission to show us just how beneficial certain worms are for our brain and gut health.
The gut microbiome is home to a rich and complex ecosystem containing bacteria, viruses, fungi, and mammalian parasites. Much like the earth’s ecosystems, industrialization, and modern lifestyles have led to a significant decline in biodiversity. Disappearing from the modern gut are helminths, parasitic worms which have been eradicated in two thirds of the global population.
While a heavy burden of worms has negative health outcomes, the surprising twist is that too few worms can also be bad for us. “Epidemiologists noticed that areas where helminths are still endemic have really low rates of autoimmune and inflammatory disorders,” Osborne explains. “Where helminths have been eradicated, those diseases are on the rise.” A possible explanation for this trend is the “Old Friends hypothesis,” which suggests that exposure to specific viruses, bacteria, and even worms during development helps build resilient immune systems.
The theory that helminth infection could be protective against certain diseases is supported by the immunomodulatory mechanisms of helminths. “Worms are powerful immunomodulators,” says Osborne. “They guide wound healing and limit inflammation, which is directly antagonistic to the damage caused by autoimmune disorders.” This is beneficial for helminths, as limiting inflammation prevents them from being expelled by the body.
Osborne’s research team investigates helminth infection in cases of multiple sclerosis (MS), an incurable autoimmune disease. In a mouse model of MS, Osborne’s lab showed that helminth infection can delay onset and promote disease remission. A recent preliminary clinical trial in England treated MS patients with hookworms, a type of helminth. It showed promising results and no adverse side effects.
Are worms the future of treating diseases like MS? “I really do believe that worms are an incredible tool for learning about the gut-brain axis,” says Osborne. But she cautions that worms are still parasites and harnessing the power of helminths may be better approached indirectly. “Perhaps there are specific compounds we can isolate from these worms that then guide immune based treatments.”
Common herbicide affects mouse behaviour
Jacqueline Barnett’s Favourite Brain Foods: Chocolate and coffee (for their impact on mood)
The food we eat impacts our brain and gut health. But how we grow what we eat matters just as much. Jacqueline Barnett (BSc’17) is a PhD candidate in Dr. Deanna Gibson’s lab in the Department of Biochemistry and Molecular Biology at UBC Okanagan. Her research investigates the impact of the herbicide glyphosate on our gut microbiome.
Glyphosate is the active ingredient in Roundup™, an agrochemical that first came on the market in the 1970s and revolutionized farming by controlling weed growth. Almost 19 billion pounds of Roundup™ has been sprayed globally since 1974, with notably high amounts used on Canadian dietary staples such as wheat, soy, oats, and corn.
Humans do not possess the pathway that glyphosate acts on, so it was believed that the herbicide did not pose a risk to human health. However, glyphosate does alter the bacteria in our gut. Glyphosate actually inhibits a really important bacterial pathway,” says Barnett. This is the shikimate pathway, a metabolic pathway used by bacteria and plants.
Opportunistic pathogens are more resistant than healthy microbes to the effects of glyphosate, which can result in the overgrowth of harmful bacteria. An imbalance in the ratio of healthy to harmful bacteria in the gut can induce an inflammatory state called dysbiosis, which has the potential to impact behaviour via the gut-brain axis.
Barnett investigated the impact of glyphosate on microbiome dysfunction and behaviour by exposing mice to glyphosate in doses approved by the Environmental Protection Agency. Her findings suggest that even the approved dose has an impact and that the effects persist through multiple generations. “We’re seeing behavioural differences – mice whose grandparents were exposed travel less and move more slowly,” she says. Glyphosate exposure also shows effects on anxiety and working memory. Research efforts to understand the impact of glyphosate on human health are growing. “It’s possible that the impact of glyphosate [has] been going on for years, but the chronic effects are compounding with subsequent generations,” says Barnett.
Barnett emphasizes that glyphosate has legitimate benefits. “We live in a world where food insecurity is a real threat,” she says, pointing to the fact that agrochemicals increase yield and reduce cost to farmers. But she hopes for better surveillance. “The Canadian Food Inspection Agency does not test for glyphosate,” says Barnett, proposing better quantification of maximum residue limits.