The Walking Wounded
Five years after the fall of Saigon to the Viet Cong on April 30, 1975, Dr. Soma Ganesan finally escaped his communist oppressors.
At the time of the takeover, which marked the end of the Vietnam War, Ganesan was employed at Saigon Children’s Hospital as a pediatrician. The victors allowed him to continue his work there. However, little else about his life remained the same.
Ganesan and his colleagues were subjected to hostile interrogation sessions at varying times of the night. On weekends, they were sent to a prison camp for “re-education,” consisting of beatings and “traction,” which Ganesan refuses to detail. The torture damaged his spine – how severely, he would only find out later. He endured by focusing on day-by‑day survival and adopting a valiant stoicism: “If you have pain, so what?”
Daniela Jorge Ayoub is a governance and policy associate at the International Rehabilitation Council for Torture Victims in Copenhagen, Denmark. How Western nations can best respond to the torture crisis, she says, is to uphold their responsibilities under the United Nations Convention Against Torture. (Canada ratified the treaty in 1987.) This includes upholding torture victims’ right to “full rehabilitation.” However, she adds, a political backlash in places like the US, UK, France, Austria and other European countries (all treaty signatories) means that nations are shirking their international obligations. “The rehabilitation sector is absolutely in a financial crisis,” Ayoub says. Policies supporting refugees and migrants “are seen as liberal and therefore automatically rejected. It’s a dangerous trend of right-wing governments.”
Canada’s record of supporting its obligations under the treaty is spotty. VAST almost shut down in 2014, when the federal Conservative Party withdrew nearly $300,000 in funding. Executive director Frank Cohn, BA’00, says that such near misses indicate the organization needs to expand its funding sources. (The provincial government currently funds two-thirds of VAST’s operations.) The specialized counselling provided to survivors of torture through VAST is vital to ensure individuals who have suffered trauma “settle in Canada in healthy and supported ways,” says Cohn. Conventional mental health supports in BC, he adds, are “unsuitable or inadequate [for] this population.”
Ganesan retires from VGH’s Cross-Cultural Psychiatry Clinic on June 30, freeing him from the administrative task of overseeing a 150-strong cohort of psychiatrists. He will be able to focus solely on counselling at CHAKRA and VAST, joining forces with Dr. Rahul Soma, his psychiatrist son. Soma spends half a day every week counselling patients at VAST, in addition to work at VGH’s Cross-Cultural Psychiatry Clinic. One of the things that drew Soma to psychiatry was his father’s devotion to helping others. “When we were growing up, we were always encouraged to help people, and I think that that had a lot to do with where my parents came from and the struggles they went through. They were always genuine, kind people and I think that had a huge impact.”
Kindness and compassion provide a strong foundation for effective therapies that help heal the wounds – invisible and visible – inflicted by malevolent forces upon human beings. With Ganesan, that kindness is rooted in an empathy reinforced by shared experience. He understands that “scars heal, but the psychological part – the deprivation of basic freedom – lasts forever, until that person dies.”
Ganesan speaks for all those people who arrive at the doors of VAST: damaged, wounded and fearful, yet emboldened by hope and determination. Shimi Kang says such qualities have the potential to elevate them beyond mere survival to thriving and taking on positions of leadership in their community. One example is Ganesan himself, whose wretched experiences in the Vietnamese prison camps, while almost breaking him physically, galvanized a career in a unique offshoot of psychiatry that helps patients understand that to be human and alive means having the capacity for renewal, no matter how horrifying the past.
The hundreds of thousands of people who underwent “re‑education” coped with starvation rations, poor sanitation and disease. They were forced to construct barracks, dig wells, cut trees and sweep minefields. The worst thing, Ganesan recalls, was not the torture so much as “the constant fear that your life is in danger, the lack of freedom of communication and expression, the witnessing of people being killed, tortured and mistreated.”
Ganesan contrived an escape. He was born in Vietnam, but his father, Sundaram Soma, who died when Ganesan was five, had emigrated from India to work in Saigon at the Indian consulate. Out of desperation, Ganesan approached the consulate office to request documents giving him official foreigner’s status. The consulate granted him the papers, and the Vietnamese regime reacted quickly, bustling Ganesan onto a plane for Singapore. It was freedom, but a gut-wrenching one – Ganesan had to leave his grandmother, mother and sister behind in Saigon.
The worst thing, Ganesan recalls, was not the torture so much as “the constant fear that your life is in danger, the lack of freedom of communication and expression, the witnessing of people being killed, tortured and mistreated.”
Still, landing on Singapore soil was like a rebirth. Having no food or a place to stay, Ganesan wandered into a park and sat down on an empty bench. Having been in a state of extreme sleep deprivation for the past five years under his communist oppressors, the quiet green park was heavenly. He lay down. “I slept for three days and three nights without food. I had never felt so peaceful in my life.”
Ganesan became an asylum seeker in India and then France, where he applied to Canada as a refugee. He arrived here in 1981, in his thirties, unable to speak English. He mastered the language, brought his family to Canada from Vietnam, and re-qualified as a physician. But pediatrics no longer appealed to him. Instead, he entered a psychiatry residency at UBC, with the idea that he could help others who had undergone similar experiences. His mother, Manh Duong, wept at the decision. “She said she was worried that people who practiced psychiatry would become nuts themselves,” he says, chuckling.
On the surface, at least, Ganesan’s life appeared to be back on track. During his second year of residency, however, he suddenly found himself unable to walk. An MRI scan showed calcification and lower-lumbar stenosis, which is when the spinal canal, which protects the spinal cord, narrows. The incredulous emergency doctor told him that only sustained severe abuse could cause such physical degradation.
Ganesan regained his mobility with therapy, although his gait is stiff – almost ungainly. Other effects of the torture still haunt him. When asleep, he is “always on alert” – perfectly lucid if someone telephones late in the night, the result, he says, of being woken for interrogation. Complete rest and repose will forever remain an abstract notion. “I keep an ear in my brain open for anything and everything.”
Ganesan realized back in the 1980s that specialized support was needed when BC took in Central American refugees from El Salvador, Guatemala and Honduras who were fleeing war and torture under military dictatorships. The existing provincial medical services could not deal with the constellation of psychological, social, physical and economic challenges these shell-shocked people were suffering.
In 1986, with support from Amnesty International and with funding from the Office of the United Nations High Commissioner for Refugees (UNHCR), Ganesan co-created the Vancouver Association for the Survivors of Torture (VAST). Two years later, he founded and led the Cross‑Cultural Psychiatry Clinic at Vancouver General Hospital (VGH), which provides immigrants and refugees from non-English-speaking nations with culturally sensitive and language-specific assessment and treatment.
Ganesan currently devotes his time to VAST as well as the CHAKRA Health Centre, a Vancouver facility he started last year for those dealing with trauma. His clients come to him for help dealing with debilitating headaches, panic attacks, insomnia, depression, and eating disorders that are rooted in the past. Known as post-traumatic stress disorder (PTSD), such symptoms can arise out of the blue, years, or even decades, after events. “Nightmares – it happens to all of us,” he says. “I’m still seeing people who survived [German] concentration camps; they are in their 80s and 90s.” One of Ganesan’s friends, who worked alongside him in the hospital in Saigon, recently started experiencing nightmares stemming from that dark period. The colleague was forced to witness prisoner executions, then had to check the bodies with a stethoscope to ensure the heart had stopped. “He is 89 and he has had to start talking to me. It’s not easy,” says Ganesan, who has the curious habit of closing his eyes when he speaks, as if shuttering his mind to his own harrowing past.
His clients come to him for help dealing with debilitating headaches, panic attacks, insomnia, depression, and eating disorders that are rooted in the past. Known as post‑traumatic stress disorder (PTSD), such symptoms can arise out of the blue, years, or even decades, after events.
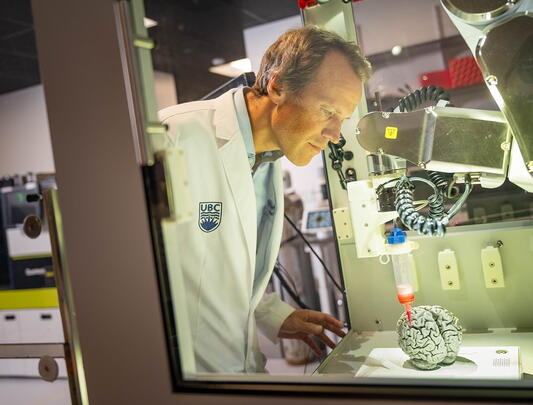
Throughout his career, Ganesan has worked relentlessly to communicate to the medical community his unique insights into the treatment of torture victims, advocating for more nuanced and sophisticated therapies. Thanks to him, UBC’s Department of Psychiatry, where he is a clinical professor, added trauma and cultural psychiatry to its curriculum in 1988. In 1995, he founded the annual Cross Cultural Mental Health Conference in order to enlighten a wide range of medical specialists, from dermatologists to cardiologists, about the perplexing connections between past trauma and current maladies, such as physical pain, addiction and mental health challenges. (Now on hiatus, the conference will resume in 2019.)
Psychiatrist and best-selling author Dr. Shimi Kang says that before the conference there was “no conversation” about trauma’s mind-body connection. Kang, who was one of Ganesan’s students and a volunteer at VAST during her UBC psychiatry training, recalls watching in awe as Ganesan gently helped a patient unravel their history of torture and trauma. Now a UBC clinical associate professor, Kang has drawn upon her experiences with Ganesan to counsel patients in her own practice, from child soldiers in Africa who had been forced to torture others to refugees from India who had been caught up in that country’s secession-related insurgencies. “Dr. Ganesan really was a leader not just in psychiatry but medicine,” she says.
Over the years, the need for trauma counselling for newcomers to Metro Vancouver has increased in tandem with escalating violence and terrorism – including targeted attacks on civilians – in areas of the Middle East, Central and South Asia, and Africa.
Statistics bear out how dark and violent the world has become for millions of people. The 2017 Global Trends report, published by the United Nations Refugee Agency (UNHCR), put the total number of refugees seeking safety across international borders at 22.5 million, which is the highest number since the agency was founded in 1950 in the aftermath of the Second World War. Syria accounted for the most refugees: 5.5 million in 2016 (and 12 million in total since the conflict began in 2011, or 65 percent of the population). Widespread conflict in South Sudan, Colombia, Afghanistan and Iraq also spawned millions of refugees. Another UNHCR report from 2017, Torture Victims in the Context of Migration: Identification, Redress and Rehabilitation, reports that five to 35 percent of refugees are survivors of torture. Not only have they fled abuse but they are also at high risk of being tortured while fleeing, enduring “beatings and starvation, sexual violence [and] arbitrary and violent detention.”